Tamil Nadu Medical Services Corporation: A Success Story
Tamil Naduís efficient drug procurement system offers clues to fixing the glitches in the national health system
It is five in the evening, but patients are still making a beeline to see Dr. N. Vijayalaxmi, the duty doctor at the district headquarters hospital at Thiruvallur, about 50 km from Chennai. The doctor patiently listens to each one of them, chides some for not coming in earlier in spite of fever, and furiously scribbles tests and medicines.
Although the hospital lacks the spiffy look of private institutions, it treats about 1,500-2,000 patients a day. “The number of patients has at least doubled,’’ says Dr. Vijayalaxmi, who joined the hospital four years ago. There are only about three doctors on duty at any given point of time.
Though the hospital staffing has not kept pace with the increase in the number of patients, she does not recall a single instance during those years when the hospital has been short of medicines. Over the years, it has also acquired modern equipment such as a CT scanner, nebulisers and those used in physiotherapy.
“Sometimes we get referrals from even private hospitals here,’’ the amiable doctor says with visible pride.
The Thiruvallur hospital is not an isolated case of a well-functioning public health care system. Tamil Nadu boasts of the best public health care system in the country. State care is so competitive that until some time ago, deliveries in private hospitals in Chennai city often cost less than those in rural Bihar. At about 9 percent of its health budget, Tamil Nadu spends the most on drugs among states. Its per capita drug allocation in 2006-2007 was Rs. 27. In comparison, Rajasthan’s was Rs. 2 in 2005-2006 and Uttar Pradesh’s was Rs. 3. Even Kerala, which boasts of reasonably robust public health care, spent only 1.5 percent of its health budget on drugs.
One of the pillars of this successful system is the Tamil Nadu Medical Services Corporation (TNMSC), a state-owned company set up under the Companies Act in 1994 in the wake of a spurious drugs scam. The corporation streamlined drug procurement in the state and has helped shave costs by about 30 percent.
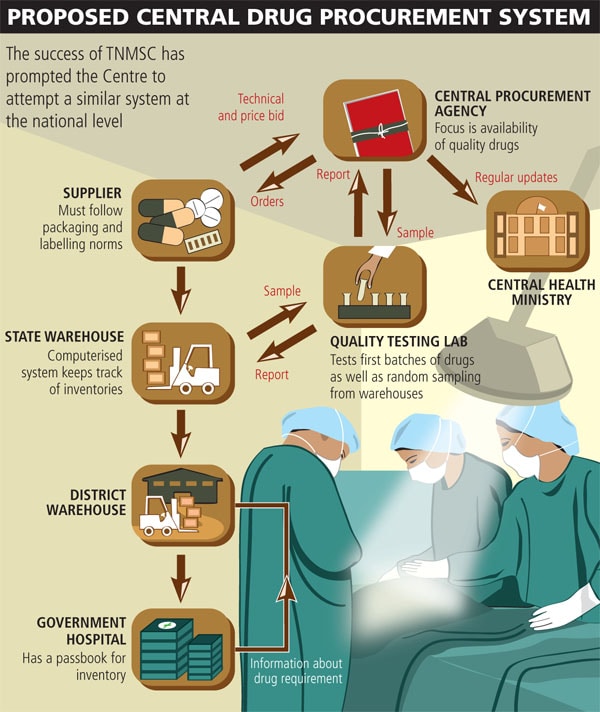
“TNMSC has a simple goal,’’ says R. Poornalingam, who set the company up. “It has to ensure availability of quality drugs to everyone at an affordable cost.’’ The central government is now using the TNMSC model as a national benchmark in rational use of drugs in the public sector in procuring, logistics and capacity building. The ministry has also proposed a company for the central government to manage the supply chain of centrally administered programmes such as malaria and TB eradication, pulse polio and HIV control. It has roped in Poornalingam as the chief evangelist for the project.
The Model
When TNMSC was set up, drug procurement in the state was scattered, with each public hospital sourcing drugs on its own with no standard procedures. TNMSC, which relied heavily on information technology systems and processes to streamline drug procurement, helped in dramatically bringing down drug prices. For instance, the price of 10 strips of antibiotic ciprofloxacin tablets in 1992-1994 (before TNMSC) was Rs. 525. That fell to Rs. 88 in 2002-2003. Similarly, the cost of 100 Norfloxacin tablets fell from Rs. 290 to Rs. 51.30 during the same period.