The 3D fine print
3D printing is making advances in health care by preparing doctors for complicated cases and customising solutions for patients. But there's a long way to go before it becomes the standard procedure f


 An artificial femur
An artificial femur
Image: ShutterstockIn February 2015, Dr Swati Garekar, a paediatric cardiologist at Fortis Hospital in Mumbai’s Mulund, was tied in knots over a 9-month-old with an abnormal hole in the heart. The child, the son of a policeman from Nagpur, had DORV (double outlet right ventricle), a congenital heart condition in which two big arteries emerged out of the right ventricle of the heart, instead of one each from the right and the left. It led to pure and impure blood getting mixed and required a complex surgical fix. But neither an echocardiogram nor a CT scan could give Garekar a detailed picture of the mess inside the heart that would barely be bigger than the baby’s fist. “Which way would the surgeon go in? What should be the best procedure? Say, we open up the patient, put him on bypass, reach his heart and see that the insides are not what we thought?” asks Garekar.
The team, including paediatric cardiac and transplant surgeon Dr Vijay Agarwal and cardiac imaging consultant Dr Alpa Bharati, grappled with uncertainty over whether to hit the operation theatre blind. Garekar says she was reminded of some cases in European hospitals where the doctors took CT/MRI scans and printed them out in 3D. Imagine holding a replica of the heart, prising open its chambers, feeling its arteries and anomalies and charting out the path of blood flow, without having to cut open the patient. “I started flipping the Yellow Pages and found a company that can print a 3D model,” says Garekar. In June, the baby was successfully operated upon, as Agarwal, confident of the anatomy after studying a 3D model in sandstone, channelled the artery from the right ventricle to the left through the hole in the heart.
While this infant’s case is reported as a first for cardiac 3D printing in India, in the three years since, a lot more is being heard about how the medical fraternity is notching up milestones. Ever since his first surgery with a 3D print in 2015, Agarwal, now with Fortis Gurugram, has studied at least 50 such models before making that nick on the chest. In February 2017, surgeons at Medanta-The Medicity in Gurugram replaced the second and the third vertebrae of a 32-year-old woman, damaged by tuberculosis of the spine, with a titanium 3D printed one. The surgery was the first of its kind in India and among the earliest in the world, with only China and Australia reporting a case each before. According to reports in the media, this April, doctors at AIIMS, Delhi, conducted an eight-hour surgery on a 40-year-old patient, to perform a complex hip replacement with a 3D printed implant. Says Firoza Kothari, the co-founder and CTO of Anatomiz3D, which 3D printed the heart model at Fortis, “In 2015, when we started, we would get about one print order a month. Now, it goes up to 40.”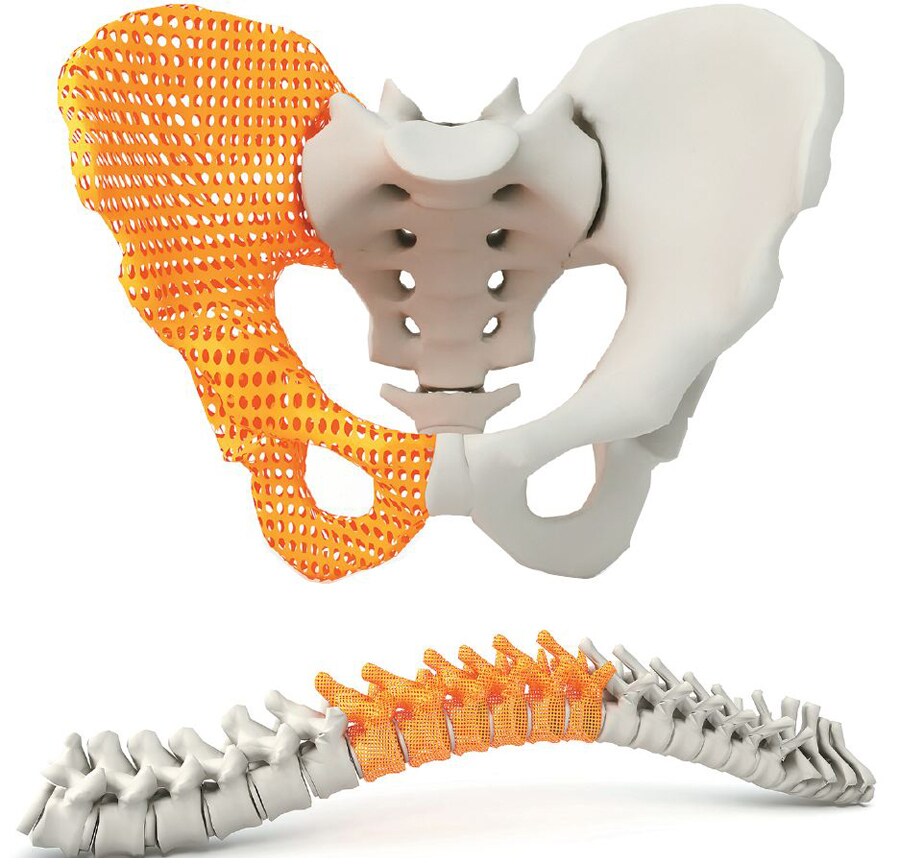 A 3D printed hip bone implant a 3D printed spinal implant
A 3D printed hip bone implant a 3D printed spinal implant
Image: ShutterstockHealth care apart, the country too can be seen warming up to 3D printing in general. According to a 2015 report by 6Wresearch, a global market research and consulting firm, India’s 3D printing market is projected to be worth $79 million by 2021, with low cost of manufacturing, increasing penetration across various applications, and its Make in India initiative spurring the rise. While the automotive sector accounts for the largest revenue and volume share, medical is seen as an area exhibiting “promising growth”. “In 2016, when we started our medical division, we got three to four cases a year. We had to run after doctors trying to understand the need and convince them about 3D printing. But since then, we’ve worked with over 50 doctors covering 100 specialisations,” says Atit Kothari, part of the leadership team at Imaginarium, a 3D printing company based in Mumbai.
TAILOR-MADE SOLUTIONS
The input data for a 3D print is the CT/MRI image, which is essentially multiple X-rays stacked on top of each other. These images can be combined into a virtual 3D model using specific software. The region of interest (say a bone fracture zone) can be segmented in consultation with the doctor and saved as a computer file. This file is then sent to a 3D printer, which fabricates the corresponding physical model layer by layer. “I call the 3D printer a jalebi maker. Just like the jalebi batter is piped out, here the plastic or metal comes out in the shape of a particular object,” says Dr Vaibhav Bagaria, an orthopaedic surgeon with Sir HN Reliance Foundation Hospital in Mumbai. Since one layer is added on top of another, 3D printing is often called additive manufacturing. 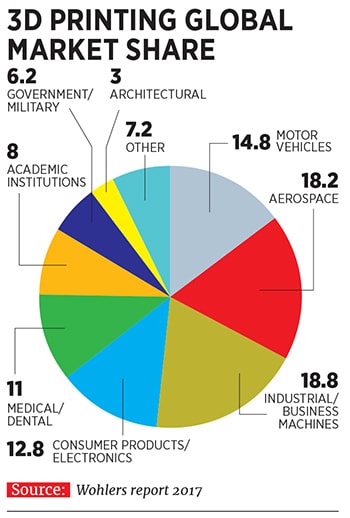 One of the reasons 3D printing is making rapid strides in medicine is that by letting doctors have a tactile feel of the anatomy and providing a spatial relationship between its constituents, it simplifies procedures and eliminates guesswork. For instance, studying the basal ganglia, the part of the brain that controls limb movements, posture etc, is now easier than doing it out of the textbook. Or the critical cranio-vertebral junction, where the skull joins the spine, with its intricate nerve structure. “India is a country that sees a lot of abnormalities in the area and each case is different. If I 3D print the area with the data of a patient, I can practise a mock-surgery and there wouldn’t be any on-table planning. That reduces complications and makes us safer doctors,” says Dr Vishwas HV, neurosurgeon and minimally invasive spine surgeon at Narayana Health City, Bengaluru.
One of the reasons 3D printing is making rapid strides in medicine is that by letting doctors have a tactile feel of the anatomy and providing a spatial relationship between its constituents, it simplifies procedures and eliminates guesswork. For instance, studying the basal ganglia, the part of the brain that controls limb movements, posture etc, is now easier than doing it out of the textbook. Or the critical cranio-vertebral junction, where the skull joins the spine, with its intricate nerve structure. “India is a country that sees a lot of abnormalities in the area and each case is different. If I 3D print the area with the data of a patient, I can practise a mock-surgery and there wouldn’t be any on-table planning. That reduces complications and makes us safer doctors,” says Dr Vishwas HV, neurosurgeon and minimally invasive spine surgeon at Narayana Health City, Bengaluru.
3D printing also helps produce cutting jigs for surgeons that factor in a patient’s anatomy to provide a ‘stencil’ for precise cuts and drills. For instance, for a mandibulectomy, a surgeon can place the jig, prepared with data from the patient’s scan, on the jaw to get exact measurements of the two ends he needs to cut to remove a tumour. “When you know what to expect, it reduces surgery time by around 25 percent,” says Dr Rajendra Nehete, a plastic surgeon at Vedant Hospital in Nashik.
3D printing also helps in rapid prototyping of tailor-made devices and implements. These can be evaluated by doctors and industry partners before they are put into final shape. Consider the reusable biopsy gun, the flexible laparoscopy instrument or the diabetic foot screener printed at IIT Bombay’s Biomedical Engineering and Technology (incubation) Centre (BETiC). With 3D printing, the institute builds prototypes of cheaper materials, like paper and plastic, through multiple iterations before moving on to expensive metal to manufacture the final product. “There are at least 30 bio-incubators in the country out of which six or seven are trying to develop medical devices. This is an exciting application for 3D printing in the years to come,” says B Ravi, the institute chair professor of mechanical engineering in IIT Bombay who also heads BETiC. Even at BETiC, about 20 percent of the 100-odd researchers and their medical and industrial partners are dedicated to developing this vertical. 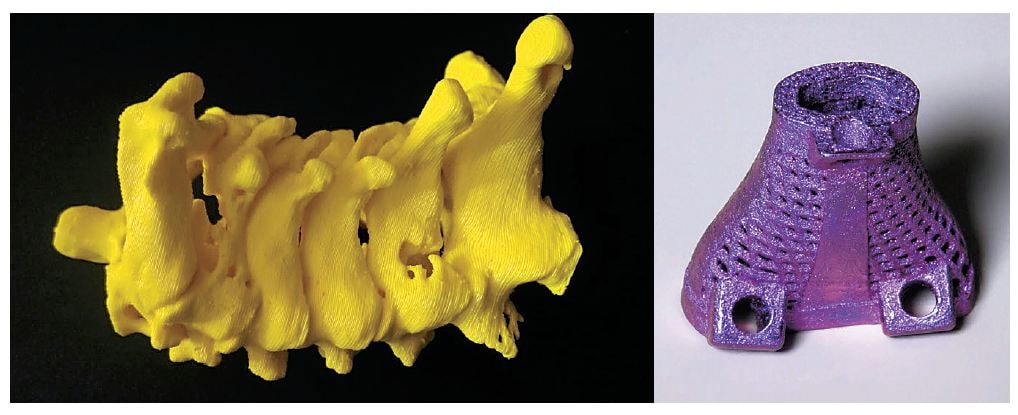 A 3D printed model of a damaged spine (left) the metal implant that it was replaced with
A 3D printed model of a damaged spine (left) the metal implant that it was replaced with
Image: Sanjay Pathak
Another application that is now taking baby steps but may surge ahead are custom-made implants. The plate to be put in difficult joints like the pelvis, the titanium mesh to cover a part of the skull created by bone removal, or spinal interbody cages in a lattice structure that fuses the implant better with the bone. “Some examples have demonstrated that mechanical properties introduced by 3D printed lattice structures remove the need for biologics such as BMP [bone morphogenetic protein] that is normally used along with a traditionally made implant in a surgery,” says Ajay Parikh, vice president & business head, Wipro 3D. 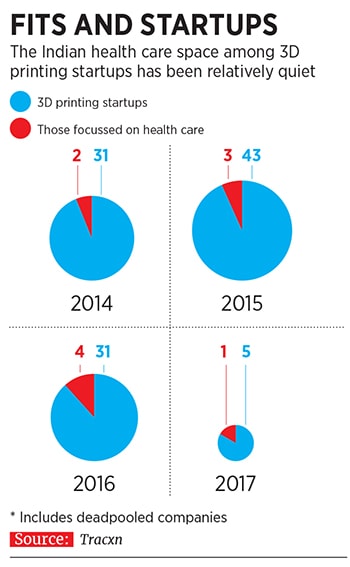 The use of implants is yet restricted to a handful of cases due to the limited availability of bio-compatible materials that won’t trigger a reaction from the body. While titanium and acrylic are the current materials of choice, the development of bone cement, radio-opaque PEEK (polyether ether ketone) and hydroxyapatite (a bone-like substance that dissolves to let human bone grow over it) are opening newer avenues. But inserting something in a human body is a tortuous procedure with multiple clinical trials, so this is a vertical that is expected to flourish with a lag.
The use of implants is yet restricted to a handful of cases due to the limited availability of bio-compatible materials that won’t trigger a reaction from the body. While titanium and acrylic are the current materials of choice, the development of bone cement, radio-opaque PEEK (polyether ether ketone) and hydroxyapatite (a bone-like substance that dissolves to let human bone grow over it) are opening newer avenues. But inserting something in a human body is a tortuous procedure with multiple clinical trials, so this is a vertical that is expected to flourish with a lag.
But once the implant business takes off, the printing companies can devise a revenue model around it, in which doctors buying implants would also end up taking anatomical models and surgical jigs to accompany the procedure of inserting those implants. Says Jitendra Singh of Imaginarium, “At present, anatomical models and surgical jigs complement each other, but once implants become more common in the industry, the rest would automatically follow.”
SLOW OFF THE BLOCKS
While the conversation around 3D printing has opened up in recent years, for nearly two decades now, India’s medical fraternity has been dabbling with it under the radar. Bagaria of Sir HN Reliance Foundation Hospital remembers a case in Nagpur about 10 years ago, where he got an engineer friend to take CT images of a patient with a complex hip injury, turn them into mechanical drawings, feed those into a CAD software and take 3D prints. “At that time, we weren’t even aware of the terminology of 3D printing, we used to call it rapid prototyping. Once it came out well, we filed a patent for converting Dicom images into a 3D printing format,” says Bagaria.
But, according to IIT Bombay’s Ravi, 3D printing made its debut with the medical fraternity even earlier, in 2002. He recalls the first time a doctor, ortho-oncologist Dr Manish Agarwal (now at Mumbai’s PD Hinduja Hospital), approached him to 3D print the pelvic bone of a 50-year-old patient with a malignant tumour in that area. The institute had bought a 3D printer in 1997, one of the earliest ones in the country.
“The pelvic bone, of which Dr Agarwal had to remove a part, is where the hip joint sits. When you remove the bone, you can’t put a normal hip joint, you need to put a custom implant. But the saddle portion of the implant has to match with the cut portion of the bone and you need to fix its shape and dimensions before the surgery. We got the CT scan images and reconstructed the 3D model on the computer. Based on Dr Agarwal’s inputs, we worked with an implant maker to fabricate a matching prosthesis,” says Ravi. The surgery was a success, but, surprisingly, 3D printing in health care didn’t take off with it. The IIT team, though, kept at it by taking up a few cases a year.One of the principal impediments then was prohibitive costs. The 3D printer that IIT bought in 1997 cost about ₹30 lakh and the model it printed for Agarwal in 2002 came for over ₹50,000. Now, a printer with similar capabilities costs less than ₹10 lakh and the bone model less than ₹5,000. The drop in prices that has caused a spurt in 3D printing has been triggered by competition and expiry of patents. In 2009, the patent on a primitive form of 3D printing, fused deposition modelling, expired, as did patents on technologies like laser sintering in 2014, bringing down prices on ‘hobby’ desktop printers to as less as ₹20,000. Besides, more companies coming into the business brought in competition. According to the Wohlers Report 2018, the number of companies selling industrial 3D printing machines globally has risen to 135 in 2017 from 97 in 2016.
However, the drop in prices is still relative to the figures a decade ago. 3D printers that can prepare simple anatomical models start from ₹1 lakh and those printing implants with bio-compatible materials could go up to a few crores. And, says Sanjay Pathak, director of Global Healthcare, the Delhi company that made the spinal implant, there isn’t much chance that price of implants, too, will plummet considerably. “Implant pricing globally is $30,000 to $35,000 for big anatomical parts like hips. In India, we do it for less than $10,000, the cheapest in the world, due to lower labour costs. Smaller implants are $10,000 to $15,000. But, in India, we do it in the range of $2,000 to $2,500.”  3D printed models, surgical jigs, braces and implants on display at the Imaginarium office
3D printed models, surgical jigs, braces and implants on display at the Imaginarium office
Image: Mexy Xavier
Besides, due to the premium placed on customisations, 3D printed models, prosthetics or implants would still be more expensive than traditionally manufactured ones. While the cost of 3D printing is becoming more and more competitive for small production runs of standard implants and prosthetics—like a lightweight plastic brace costing up to ₹8,000 or the model of a simple fracture between ₹3,000 and ₹5,000—the 3D model of a heart would come for anything between ₹18,000 and ₹30,000 and a titanium cranial implant between ₹60,000 and ₹1.5 lakh.
3D printing has also come up short when it comes to matching mass-scaled prosthetics like the Jaipur Foot. The socket in the prosthetic knee on which the foot sits takes far longer to print than those manufactured traditionally, and does not have the strength to bear the weight of the amputee. “It’s a great technology for prototyping, but has limited use for implants needing strength,” says DR Mehta, founder and chief patron of the Bhagwan Mahaveer Viklang Sahayata Samiti, which makes the Jaipur Foot. Ravi admits that while a 3D printed socket fabrication did enhance accuracy, it takes close to 24 hours and turns out far more expensive. IIT-Bombay is now trying to evolve another method based on the CNC machining of sockets that would be faster than conventional methods and would be priced more competitively.
In some cases, doctors have found a way of going around the expenses. Garekar at Fortis and the consultant paediatric surgeon there, Dr Dhananjay Malankar, recall a case in which a three-year-old Nigerian with DORV was wheeled in. Neither Garekar nor Malankar were certain about the case even after an echocardiogram and the family didn’t have enough money to pay for a 3D scan. So, she got Anatomiz3D to share pre-printed computer visuals, which were less expensive than a 3D printed model. “Usually, unless you are sure with DORV patients, you don’t know what to open: The right atrium, the right ventricle, the pulmonary artery or the aorta. But the 3D view gave us a plan and we opened up the right atrium and the right ventricle. The surgery turned out to be good and the patient was discharged in a week, the time usually taken for routine cases,” says Malankar.
This is the narrative that the 3D printing companies are banking on. Says Kothari of Anatomiz3D, “OT hours, long discharge time plus blood loss and chances of complications are all reduced if the doctor is more informed about a surgery with the real-feel of a 3D model. All these factors would eventually rationalise the costs.”
What causes a further setback for medical expenses is that 3D printing isn’t yet covered by organised insurance. For that to happen, it would require regulatory supervision to ensure standardisation of procedures and quality control of the printing units. “That will happen once it moves from being a niche product to a more prevalent practice. It will also need new product liability and professional indemnity covers besides specific actuarial interventions for the insurance companies,” says Samir Bali, a senior management consulting and insurtech professional. Eventually, 3D printing will make medical procedures more time-efficient (by improving planning and reducing overheads) and cost-efficient (when implants are produced at a scale), and insurance companies will recognise the significant advantage accruing to them, Bali adds.
IS THE FUTURE HERE?
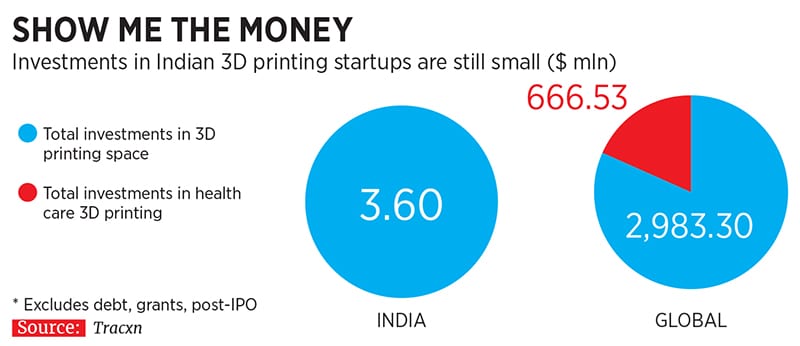
Perhaps because the 3D health care industry is still counting down to a take-off, one has barely seen any funding in startups since 2014 (till 2017). Data from Tracxn shows that while about 40-odd 3D printing startups have mushroomed every year since 2014, those focussed on health care remain in single digits. During that period, while the startups have raised $3.60 million through nine rounds of funding, not a single penny in venture capital (VC) has come in for the health care ones. 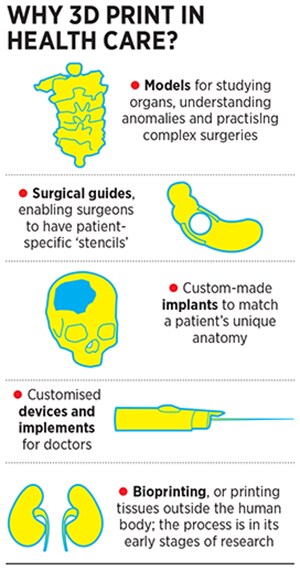 “Given their limited constituency, these startups may not feel the need to raise crores from VCs to scale up. Like traditional businesses, they can grow to ₹5 crore to ₹10 crore or ₹20 crore. But that may not be the scale in which VCs may be interested,” says Dr Ramesh Byrapaneni, a cardiologist-turned-VC who is now the managing director of Endiya Partners.
“Given their limited constituency, these startups may not feel the need to raise crores from VCs to scale up. Like traditional businesses, they can grow to ₹5 crore to ₹10 crore or ₹20 crore. But that may not be the scale in which VCs may be interested,” says Dr Ramesh Byrapaneni, a cardiologist-turned-VC who is now the managing director of Endiya Partners.
One exception would be Bengaluru-based Pandorum Technologies, the first Indian company to 3D print a liver tissue. In February, Pandorum raised about ₹23 crore in a Series A round from investors like the Indian Angel Network, 021 Capital, existing investor Binny Bansal and Hero Enterprise Chairman Sunil Munjal (own capacity). But co-founders Arun Chandru and Tuhin Bhowmick refuse to be called a 3D printing firm. “3D printing is a popular word. But it’s just one of the tools we use. Our work is in tissue engineering and regenerative medicine, a much broader field. We work on bio-engineered liver and cornea, with the final goal to develop them as lab-grown transplantable tissues,” says Bhowmick.
In 2015, Pandorum developed its first 3D mini liver tissue. The company can generate such tissues that comprise 10,000 to 1 million cells. But it may take about five years to build the working prototype of a tissue that has billions of cells and can be transplanted into a patient. Such a tissue will need to have its own blood vessel structure and be able to integrate within the receiver’s body this will require multiple trials before it can be even deemed fit for human use. “Right now, the mini-liver tissue reflect the characteristics of those grown within the human body. So pharma companies can test the hepatotoxicity of drugs, or FMCG companies their products, nixing the need for animal trials,” says Chandru.
The world is now experimenting with the endless possibilities of bioprinting, or the 3D printing of living cells. In May 2017, researchers were able to restore fertility in mice with bioprinted ovaries. Says Gordon Wallace, the director of the Intelligent Polymer Research Institute, University of Wollongong, Australia, and the co-author of an ebook on bioprinting, “The versatility in the arrangement of composition and bioactive entities in 3D printed structures means we have an effective approach to tissue/organ repair. So we are currently learning how to print systems that facilitate the growth of bits of organs. Surely, one day, that knowledge will morph into an ability to create complete organs.”
But what is a realistic timeframe to figure out if this final frontier can be breached? “If I have to bid a number I would possibly say 10 to 20 years. But five years ago, we didn’t think we would be having a conversation about printing stem cells. So who knows what the future holds?”
First Published: Sep 18, 2018, 18:23
Subscribe Now